Organisations’ Roles and Responsibilities
The health of people in contact with probation is a complex issue, crossing boundaries between health, social care and criminal justice organisations. Moreover, health status is related to other wider determinants of health such as housing and employment. Consequently, addressing the health needs of people in contact with probation supports meeting the aims and objectives set out in policy for health, social care and criminal justice agencies. It contributes to reducing health inequalities, reducing re-offending and building safer communities.
It would not be possible or helpful to attempt to describe all relevant national and local level policies here. Consequently, we have simply set out to summarise the roles and responsibilities of different organisations across the health and justice sectors in England as they are set out in policy.
It is also important to note that communication and information sharing between these different agencies is key in order to support the individual and achieve continuity of care.
The Role of Clinical Commissioning Groups (CCGs)
• Responsible for commissioning healthcare services for offenders being managed in the community (rather than in secure environments which are the responsibility of NHS England). This includes those in contact with probation services (Crime and Disorder Act Section 39 (1) 1998, NHS England 2016, NHS England 2017: 11). This includes provision for Mental Health Treatment Requirements (NOMS undated)
• Expected to assess the healthcare needs of their local population by working with local Health and Wellbeing Boards (an executive decision-making body headed by a committee of the local authority) to develop a Joint Strategic Needs Assessment and Joint Health and Wellbeing Strategy (see below for more on this)
• Required to be part of statutory Community Safety Partnerships consisting of the local authority, police, fire and rescue service, Community Rehabilitation Companies, National Probation Service and aim to reduce crime and disorder (Crime and Disorder Act Section 39 (1) 1998). However, a recent review by the Local Government Association (2018) points to “a mixed picture in engagement by clinical commissioning groups (CCGs) and probation services, despite their statutory obligations” (Local Government Association 2018: 10)
• Have a role to play in making NHS staff available to assess people who may benefit from a Mental Health Treatment Requirement (MHTR) (NOMS undated)
• “Should work to ensure that GP registration is promoted with offenders in the community and that GP practices provide such mental health treatment, dependent on local provision, as may be specified in an MHTR and available at a given GP Practice. Health commissioners should seek to ensure that offenders are not excluded from accessing services and ideally ensure offender mental health treatment is explicitly detailed in contracts” (NOMS undated: 11)
The Role of NHS England
NHS England has a budget of over £100 billion to commission organisations to provide healthcare services. They commission primary care services such as GPs and dental services as well as selected specialised hospital services for the general population.
In relation to offenders, the Health and Justice Teams in NHS England commission health services in secure settings including:
• Public sector prisons
• Youth detention centres
• Secure settings for children and young people
• Immigration and detention and removal centres
• Sexual assault referral centres
• Criminal justice liaison and diversion services
NHS England are not responsible for commissioning health services for people in contact with probation (see the CCG and Public Health entries for more on this). However, in Strategic Direction for Health Services in the Justice System 2016-2020 (NHS England, 2016) the government sets out its ambition to “narrow the gap between those in criminal justice and detained settings and the rest of the population in terms of health and care outcomes” (NHS England 2016: 10) and ensure continuity of care post-release. It states that “commissioners and providers need to work together to identify individuals with unmet needs across every setting at the earliest possible point to ensure that children, young people and adults receive timely, person-centred care which takes a holistic view of their individual needs” (NHS England, 2016: 11).
This document also emphasises the need to focus on improving mental health, reducing substance misuse and having appropriate pathways to achieve continuity of care. In order to achieve these aims, those commissioning and providing healthcare in the community will need to liaise with NHS England and organisations across the criminal justice pathway to ensure continuity of care.
Similarly, NHS England are committed to supporting continuity of care and improving data collection and information sharing around the health of people in their care in the National Partnership Agreement for Prison Healthcare in England 2018-2021 (HM Government and NHS England 2018).
The Role of Public Health England
Public Health England (PHE) is an Executive Agency of the Department of Health. PHE exists to protect and improve the nation’s health and wellbeing and reduce health inequalities. It does this through world class science, knowledge and intelligence, advocacy, partnerships, the delivery of specialist public health services, and through providing expert advice to Government and policy makers.
Public Health England have a National Health and Justice Team that aims to:
“improve health, reduce health inequalities and drive down offending and reoffending behaviour by understanding and meeting the health and social care needs of people in contact with the criminal justice system (in custody and in the community) through collaborative work with statutory and voluntary sector partners and with service users” (Public Health England 2018: 5).
It does this through:
• Gathering and providing evidence and intelligence to inform and support the work of local and national commissioners and service providers
• Providing expertise at local and national level on a broad range of health protection, health promotion and disease prevention activities working in close partnership with local commissioners and service providers
• Supporting partners, including commissioners and providers of health and social care, in the development of care pathways which account for the movement of people around the detention estate and between prescribed detention settings and the community
• Developing the evidence-base to support commissioning and service provision through primary research, audit, collection and analysis of data, publication and dissemination of information, reports and research studies
• Identifying emerging health threats to detainees and staff working in prescribed places of detention (PPDs) and providing advice on their management or mitigation
• Leading international engagement on prison health through its work as the UK Collaborating Centre to the World Health Organisation Health in Prisons Programme (WHO HIPP) (Europe)
• Supporting collaborative working for health across the devolved administrations of the UK and with the Republic of Ireland through the Five Nations’ Health & Justice Collaboration
The Role of Her Majesty’s Prison and Probation Service (HMPPS) – National Probation Service (NPS) and Community Rehabilitation Companies (CRCs)
HMPPS is responsible for carrying out sentences given by the courts in both prison and the community and rehabilitating people in their care. They are committed to supporting continuity of care post-custody, and improving collection and sharing of data about the health of people in their care (HM Government and NHS England 2018). Good planning and communication between prisons, the NPS and CRCs at transition points is essential to ensure that people receive and engage with healthcare.
Transforming Rehabilitation, A Strategy for Reform (2013) and the Offender Rehabilitation Act (2014) introduced changes to the way that the probation part of this service is provided in England and Wales, splitting the previous service into 21 ‘Community Rehabilitation Companies’ (CRCs) that manage low-risk and medium-risk cases, and the public sector National Probation Service (NPS) that manages high-risk cases. This white paper and Act also extended probation supervision to everyone on release from prison, including those sentenced to 12 months or less (who previously would not have been managed by probation).
The role of the NPS and the CRCs in relation to the health of people on their caseloads includes:
• CRCs aiming to make the transition from prison to the community seamless through providing ‘Through the Gate’ services to prisoners. Ideally, this would include identifying a need for (continuing) health care and ensuring that arrangements are in place to facilitate this e.g. GP registration, appointments with substance misuse services
• Staff discussing offenders’ health and social care needs with them, identifying and recording health needs using tools like OASys (offender assessment system for prisons and probation services), monitoring behaviours such as patterns of substance misuse, considering the relationship between health and offending behaviour, and facilitating offenders’ access to services e.g. through increasing GP registration and partnership working (National Probation Service 2018)
• Working with local healthcare commissioners to create clear pathways into treatment for people in contact with probation and ensure that there is adequate service provision to meet their needs (National Probation Service 2018)
• Managing people’s risk of suicide and reducing the rate of self-inflicted death amongst people in contact with probation (National Probation Service 2018)
• NPS and CRC staff working in partnership with other agencies to promote offenders’ mental health needs and ensure appropriate recommendation and delivery of Alcohol Treatment Requirements, Mental Health Treatment Requirements and Drug Rehabilitation Requirements (see below)
• Work with partners to deliver the Offender Personality Disorder Pathway
Community orders with implications for health
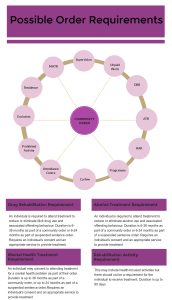
There are 12 possible requirements that can be added to a community order, some of which have a focus on health issues that may be related to or influence offending behaviour. These are highlighted in the graphic below. Some of these requirements are currently under-used. For example, despite a high prevalence of mental illness amongst people in contact with probation, mental health treatment requirements are added to a very low proportion of community orders (Khanom, Samele et al. 2009, Scott and Moffatt 2012).
Health and criminal justice agencies can improve this by working together to identify those with a mental health need. CCGs commissioning mental health services can ensure that appropriate service provision is in place to enable sentencers to have confidence in adding these requirements to community orders.
In addition, Community Sentence Treatment Requirements are being piloted in Birmingham, Plymouth, Sefton, Milton Keynes and Northampton with a view to increasing engagement with mental health, drug and alcohol treatment. The government has committed to expanding provision for this in the NHS Long Term Plan published in 2019.
The Role of Mental Health Trusts
Mental Health Trusts (or Foundation Trusts) are commissioned by Clinical Commissioning Groups to provide services for people with mental ill health. Care for offenders with mental illness is provided by forensic services at three levels of security: low, medium and high. Please see a guide here around commissioning of these services: (Joint Commissioning Panel for Mental Health 2013).
Staff from Mental Health Trusts can play a role in Multi-Agency Public Protection Arrangements (MAPPA – see later section outlining this), supporting liaison and diversion teams and the use of Mental Health Treatment Requirements as part of community sentences.
The Bradley Report was instrumental to the introduction of liaison and diversion teams, which now cover over 80% of the population in England. These services are designed to identify people with mental illness and divert them away from the criminal justice system and into treatment as and when this is appropriate. The government is aiming to ensure that they are available in all parts of the country in the near future (NHS England, 2016).
Mental Health Treatment Requirements are currently under-used (Khanom, Samele et al. 2009, Scott and Moffatt 2012), and Mental Health Trust staff can play a role in working in partnership with probation to identify people that may benefit from these requirements, and ensuring that sufficient provision is in place to enable these requirements to be used.
The Bradley Report also highlighted problems with silo working between and within health and criminal justice services, and difficulties that probation staff can encounter in managing cases with mental illness due to a lack of mental health awareness training and/or knowledge of available care pathways and how to access them. Trust staff can help to overcome these problems through working in partnership with probation, providing training and information about care pathways to probation staff.
In addition, staff from Mental Health Trusts can work alongside probation staff as part of the Offender Personality Disorder pathway (see the examples of good practice section for more about this).
The Role of Public Health Departments and Local Authorities
• Public Health departments are situated in Local Authorities and aim to improve and protect the health of the population and to reduce health inequalities. The impact of their work is monitored through the Public Health Outcomes Framework which includes indicators that are likely to have high significance to many of those in contact with probation (e.g. indicators around successful completion of drug treatment and alcohol treatment and continuity of care)
• Local Authorities have a non-mandated function as a condition of the public health grant for commissioning substance misuse services, and are an integral part of the development of Joint Strategic Needs Assessments (JSNAs) and Joint Health and Wellbeing Strategies (JHWSs) (see below for more on this) which are used to inform decisions around healthcare service commissioning in their local area (NHS England 2016)
• Local Authorities also have a duty to assess and address social care needs amongst people in contact with probation (The Care Act 2014, Social Services and Well-Being Act 2014 (Wales))
The Role of Police Crime Commissioners
All police forces in England and Wales are now represented by a Police and Crime Commissioner (PCC) apart from London and Greater Manchester where the Mayor performs this role. PCCs have been encouraged to work with health partners, including voluntarily participating in Health and Wellbeing boards. There are now many examples of joint working including (jointly) commissioning services related to substance misuse and mental health (e.g. street triage), and involvement in community partnerships for mental health and custody (e.g. the Association of Police and Crime Commissioners is a signatory to the Mental Health Crisis Care Concordat (Revolving Doors Agency 2017).
They are in a unique position to bring different agencies together to try innovative approaches to tackling issues such as substance misuse that are linked to crime in their area as described in a recent report from the Revolving Doors Agency (Revolving Doors Agency 2018).
Multi-Agency Public Protection Arrangements (MAPPA)
Current MAPPA arrangements are detailed in the Criminal Justice Act 2003. MAPPA is a process whereby agencies work together to protect people from harm by sexual and violent offenders living in the community.
MAPPA consists of:
• A ‘responsible authority’ made up of representatives from the local police, prison service and national probation service
• Representatives from agencies that have a ‘duty to co-operate’ with MAPPA, which at the time that this legislation was introduced included the local Health Authority or Strategic Health Authority, the Primary Care Trust (now Clinical Commissioning Group) and the NHS Trust
• A Strategic Management Board (which should include representatives from the ‘duty to co-operate agencies’)
• Lay advisors
A key focus of MAPPA is on information sharing between all of these agencies in relation to offenders’ risk of harm to self or others, and the recording of information on a database called ViSOR. Each Strategic Management Board will produce an information-sharing agreement, and all information-sharing must be lawful, necessary and proportionate. In some cases (depending on the outcome of risk assessments), cases may be discussed at multi-agency case meetings.
Some organisations have specific roles within this process. For example:
• Representatives from the National Probation Service must attend all Level 2 and 3 meetings
• CRC Offender Managers may also attend meetings if a case that they managed has recently been transferred due to an escalation in risk
• Health and Social Services authorities must provide after-care services to offenders subject to hospital orders under section 37 of the Mental Health Act 1983 who are discharged from hospital, for as long as they need them (National MAPPA Team 2018)
• Mental Health Services
o Must provide a consistent core representative at MAPPA meetings that can commit resources on behalf of their organisation, and may also ask relevant members of clinical teams to attend to comment on individual cases within their care
o May be required to provide clinical risk assessments or “an insight into the mental health of an offender, how it relates to risk and risk to self, and the relevant clinical interventions available” (National MAPPA Team 2018: 62). Other health professionals such as GPs may also contribute to risk assessment by sharing relevant information
o Must provide relevant information to update ViSOR cases
Joint Strategic Needs Assessments (JSNAs) and Joint Health and Wellbeing Strategies (JHWSs)
The Health and Social Care Act 2012 established Health and Wellbeing Boards to enable services to be commissioned locally to meet the needs of the local people and to reduce health inequalities. They now exist in all upper tier Local Authorities in England. Through these Boards, Local Authorities and Clinical Commissioning Groups have equal and joint responsibility to produce:
• Joint Strategic Needs Assessments (JSNAs) – assessments of current and future health and social care needs in the local population, and
• Joint Health and Wellbeing Strategies (JHWSs) – strategies for meeting the needs identified in the JSNAs
In relation to JSNAs the government stated that “each health and wellbeing board is likely to approach them according to their own local circumstances. It would not therefore be appropriate for central Government to be prescriptive about the process or to monitor the outputs (P4 Statutory Guidance 2013).
However, guidance encourages Health and Wellbeing Boards to assess the needs of disadvantaged groups that are likely to be in poor health such as offenders as part of this work. This is vital if we are serious about reducing health inequalities in society and ensuring that we have healthcare that is truly accessible to all. Indeed offenders are specifically named within the guidance as a socially excluded and vulnerable part of the population that commissioners should engage with (Department of Health 2013).
Despite this, Rebalancing Act notes that those in contact with the criminal justice system are often “not ‘visible’ in Joint Strategic Needs Assessments of Health and Wellbeing Strategies published by DsPH [Directors of Public Health] although clearly were among groups included among those experiencing health inequalities” (Revolving Doors Agency 2017: 4). Moreover, our own research showed that very few JSNAs mentioned offenders in any way and even fewer made any recommendations on how to address their health needs.
The role of organisations in commissioning healthcare for people in contact with probation is summarised below:
We would also like to acknowledge that currently many of the services that work closely with people in contact with probation are provided by the third sector – voluntary and community organisations and social enterprises.