What services are available, what should be available and how can these services best be provided?
We wanted to:
- Find out what healthcare services are currently commissioned for people in contact with probation across England
- Identify examples of good practice in delivering healthcare to people in contact with probation in a way that improves their health or access to healthcare
- Identify barriers to service access that people in contact with probation or probation staff may encounter when trying to access or facilitate access to healthcare services
- Find out what measures may ensure accessibility of healthcare for people in contact with probation
To do this, we conducted a review of the international literature from the year 2000 to May 2017. We also used a combination of surveys and freedom of information requests to Clinical Commissioning Groups, Mental Health Trusts, Public Health Departments, Community Rehabilitation Companies, the National Probation Service and probation Approved Premises to find out about what healthcare services they commission, provide or receive. Additionally, we conducted interviews with people from these organisations in six areas of England to find out about the services and/or barriers to service access in their area of the country in more detail.
Findings from the systematic review, survey work and interviews are summarised below to highlight gaps in current service provision, and recommendations for optimal commissioning strategies and potential models of good practice to improve health and access to healthcare.
Suicide
In our literature review, we identified that very little research in the UK has studied suicide and self-harm amongst people in contact with probation. However, the research that has been conducted shows that rates of suicide are higher amongst people in contact with probation than amongst the general population, and people are at particularly high risk during the weeks following release from prison.
In our case study work we identified that some areas have suicide prevention partnerships and suicide audit processes. Our review of the literature identified one study of a small sample of cases in one UK probation area which suggested that management of suicide risk could potentially be improved through:
- Targeted suicide prevention training
- Staff recognising that missed appointments could be a sign of increased risk of suicide
- Staff reviewing suicide risk when instigating breach, legal proceedings or enforcement action
- Consistent supervision by the same staff
- Using the Delius system (a system that probation staff use to record contacts with their clients) to alert others about an individual’s perceived risk of suicide (Borrill, Cook et al. 2017)
Improving access to services and continuity of care
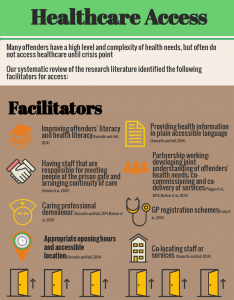
Papers included in our systematic review pointed to a number of barriers that people in contact with probation may encounter when trying to access healthcare. These are summarised in the info-graphic below.
The literature also pointed to potential ways of improving access to services to maximise good health. These are summarised in the info-graphic below.
Link to barriers info-graphic: https://my.visme.co/projects/mxnkkvy8-pmjlj0qx44qg2z39
Link to facilitators info-graphic: https://my.visme.co/projects/q6r811zr-3ezl33p8drjrl0q1
The following were also identified as barriers to service access in the interviews that we conducted in six case study areas in England:
Read more
• Behaviour difficulties: People in contact with probation displaying or being perceived as likely to display disruptive behaviour
• Complexity: People in contact with probation often have complex health problems and in addition, the healthcare system is complex to navigate
• GPs: Getting people in contact with probation registered with a GP can be problematic, particularly for people that are homeless. This in turn can cause difficulties for gaining access to other services
• Problematic referral processes: The National Probation Service and Community Rehabilitation Companies do not always have straightforward referral routes that they can use to facilitate access to healthcare for their clients. Sometimes people in contact with probation do not meet the referral criteria for services, for example, because their problems are not deemed to be severe enough, they are not resident within the correct geographical boundary to access a service, or they have a dual diagnosis
• Motivation: People in contact with probation are not always motivated to attend appointments with healthcare
• Under-use of requirements: People not having mental health, drug or alcohol treatment or rehabilitation requirements as part of their probation could also form a barrier to service access
• Risk over health: The primary focus of criminal justice staff has to be on risk management rather than assessing or addressing their clients’ health issues, so when resources are scarce, health may not be seen as a priority
• Opening hours: Services are often only open 9-5
• Difficult for some services to engage in partnership working: This was particularly apparent in relation to CCGs
So the accessibility of healthcare could be improved by increasing literacy and health literacy levels amongst people in contact with probation; providing health information in plain language to make it more accessible; having case managers meet individuals at the prison gate and monitor their access to services; criminal justice and health organisations working together to understand offenders’ health needs and provide appropriate service provision; the introduction of GP registration schemes; co-location of services or staff, and healthcare staff having a caring professional demeanour.
The government has recognised the importance of improving continuity of care, and many organisations have committed to working towards this (see for example HM Government and NHS England 2018).
The NHS Long Term Plan published in 2019 highlights that RECONNECT will be helping people to transition from prison to community based services. Similarly, work published by Public Health England highlights the value of community workers reaching into prisons and visiting prisoners prior to release in order to improve engagement with substance misuse treatment services post-release (Public Health England 2018).
Mental health
Our review of the literature suggested that having probation Approved Premises that specialise in working with people with mental illness is beneficial.
The review also identified an article about approaches to tackling the problem that people with mental illness are more likely to fail on probation supervision (defined in the literature as having an order revoked for a technical violation or a new offence (Skeem and Eno Louden 2006)). This pointed to ‘specialty probation agencies’as a potential solution to this problem and stated that they “hold promise for improving clinical and criminal outcomes for probationers and parolees with mental illness” (Skeem and Eno Louden 2006: 333). Key findings from the research about the main features of these agencies and their effectiveness are summarised below.
We also identified some other innovative practice through our case study work, and have produced info-graphics in collaboration with participants in our research and individuals involved with these services or ways of working. It is important to note that not all of these initiatives have been formally evaluated.Thus we cannot conclusively recommend them as ‘good practice’, merely as services or ways of working that were considered to be working well by participants. In some cases they are currently undergoing evaluation. Those looking to improve practice may wish to learn from these examples when considering new ways of working, but should also commission evaluation work alongside this to improve our understanding of the effectiveness of these approaches.
The first of these is the Offender Personality Disorder Pathway, which is jointly funded by HMPPS and NHS England and operates nationally. The info-graphic below provides an overview of the core aims and elements within this initiative. The info-graphic can also be viewed here: https://my.visme.co/projects/ep83k9vy-4qk5y7oz88kr5r1v. Those wishing to learn more about personality disorder may also wish to refer to Working with offenders with personality disorder. A practitioner’s guide, particularly appendix B:https://www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2015/10/work-offndrs-persnlty-disorder-oct15.pdf.
Our second example here is the service provided by Clear Counselling for Warwickshire CRC.


Substance Misuse
In our literature review, we identified a diverse range of studies on ways of addressing substance misuse problems for those in contact with probation or on parole. Much of this research consists of small-scale studies of short-term projects or initiatives and has limited generalisability. Therefore, it is difficult to draw firm conclusions in terms of what the most effective ways of providing substance misuse services to people in contact with probation are in order to improve their health and/or access to treatment.
Many substance misuse services are provided by third sector organisations. In several areas of the country substance misuse services are provided by a charity called Addaction, a service which was highlighted in our interviews. An info-graphic on this service is included below, and can also be accessed here: https://my.visme.co/projects/ep8ye6ry-z4p5zzd7qq6957n1
Similarly, Change, Grow, Live also provide services for people with substance misuse problems and were referred to by several of our interviewees. Again, it is important to note that we are not recommending these services above others, we are simply attempting to provide an overview of them that includes the positive features that were noted by participants in our case study work.
Strategic Partnership Working
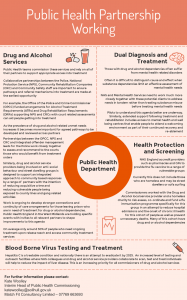
In our case study work participants described robust partnership working as a key to effective service provision. We identified a model of integrated care provision for people with drug and/or alcohol misuse problems. This is described in the info-graphic below.
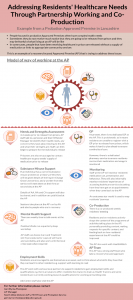
In our case study work we also identified a useful model of partnership working to address the healthcare needs of Approved Premises residents. This is described in the info graphic below, which can also be accessed here: https://my.visme.co/projects/dmvy9y07-m3x58kv13zye5krp
Our case study work also included an example of strategic partnership working by Public Health: